Introduction
Stroke management is a critical aspect of emergency medical care, where every second counts. Our Lady of the Lake Regional Medical Center (OLOL) recognized the need to enhance their stroke protocol to match the efficiency of Comprehensive Stroke Centers. This case study explores how the introduction of the Patient Transfer Scale (PTS) revolutionized their stroke management process, leading to significant improvements in treatment times and patient outcomes.
The Problem
OLOL's previous stroke alert process was inefficient, leading to delays in CT/CTA results and unnecessary patient and staff movement. The hospital aimed to streamline their process to support faster treatment times, crucial for effective stroke intervention.
Objectives
OLOL set specific goals to improve their stroke protocol:
- Decrease CT/CTA times
- Reduce stroke intervention times, including "Door to Needle" and "Door to Groin" times
- Establish a common meeting spot for stroke activation
- Minimize patient movement and wasted time
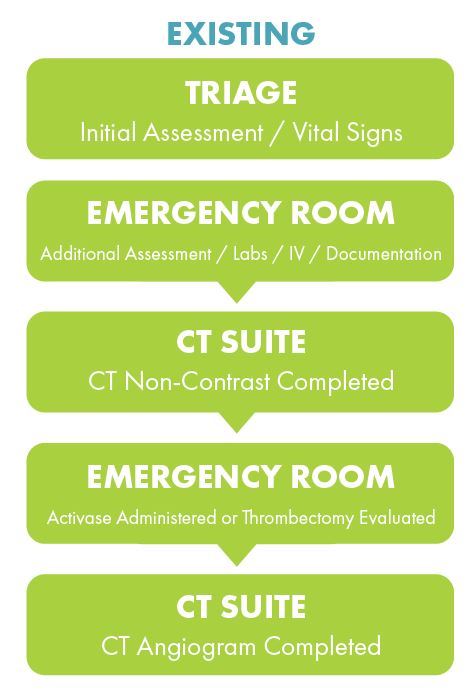
The existing stroke alert process involved multiple steps:
- Patient taken to triage for vitals and weight measurement
- Patient moved to an ED room for assessment and initial documentation
- Decision for CT made and orders entered
- Patient transferred to CT Suite for non-contrast CT
- Patient returned to ED room for treatment evaluation
- Patient transferred back to CT Suite for CT Angiogram (CTA)
Methodology
OLOL introduced four major initiatives to meet their stroke protocol goals:
- Eliminate Unnecessary Patient Movement
- Patients brought directly to the STROKE LANDING ZONE by EMS, bypassing triage and patient room.
- Team meets the patient at the STROKE LANDING ZONE, located outside the CT Suite.
- Maintain Safe Environment
- Accurate weight obtained upon transfer to CT table using the Patient Transfer Scale, eliminating the need for a weighted stretcher.
- Supplies readily available to provide efficient care.
- Leverage Multiple Disciplines
- Clinical Service Representative enters orders to help with throughput.
- Enhance Staff Communication
- CCMS APP provides guidance and contacts Neurology directly.
- Comm Techs collaborate with EMS to communicate relevant patient information to the team.
Change in Stroke Management Protocol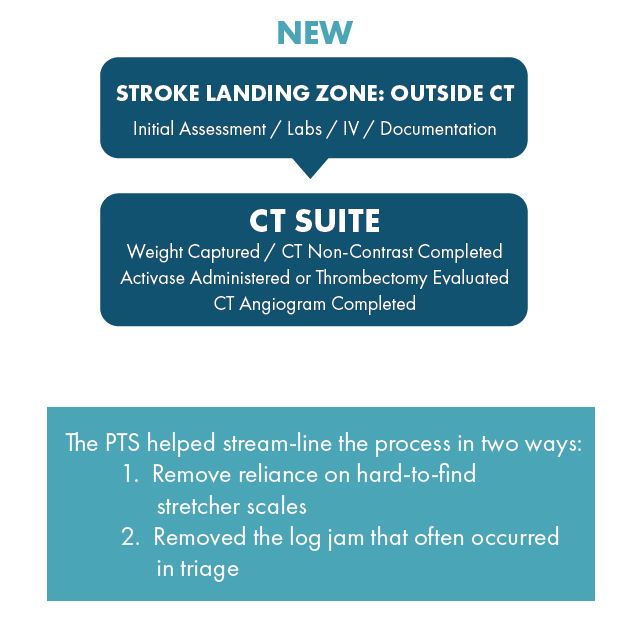
The new protocol streamlined the process by reducing the number of locations a stroke patient needed to visit:
- STROKE LANDING ZONE: Initial assessment, labs, IV, and documentation.
- CT SUITE: Weight captured, CT non-contrast completed, Activase administered or thrombectomy evaluated, and CTA completed.
Results
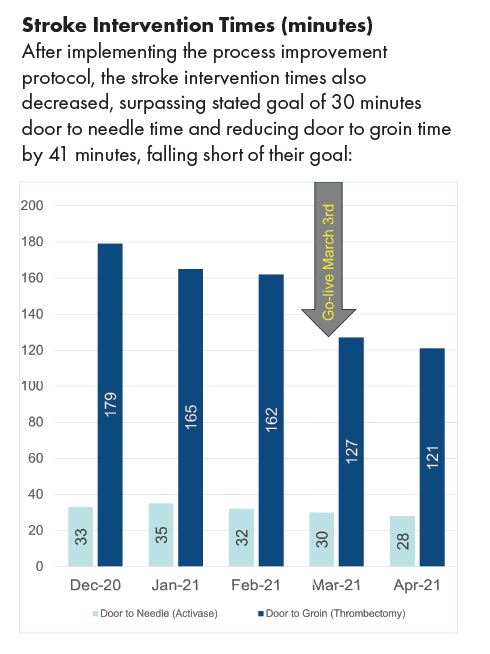
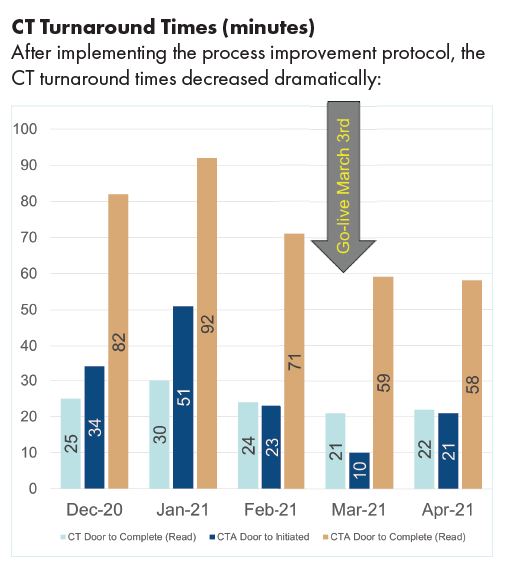
The implementation of the Patient Transfer Scale led to significant improvements:
- CT Turnaround Times: Decreased by 2 minutes.
- CTA Turnaround Times: Decreased by 23 minutes.
- Door to Needle Times: Decreased by 4 minutes, achieving the goal of sub-30-minute timeframe.
- Door to Groin Times: Decreased by 41 minutes, achieving 40% of the initial goal reduction.
By incorporating the Patient Transfer Scale into their stroke protocol, OLOL was able to support treatment times comparable to a Comprehensive Stroke Center. The PTS enabled efficient and effective stroke management, leading to increased safety, decreased likelihood of errors, better decision-making, and improved communication among the medical team.
If you would like to learn more about how the Patient Transfer Scale can help your stroke management process, visit /innovations/patient-transfer-scale/ to request a free virtual or in-person demonstration.